We present a case of partial obstruction of the third portion of the duodenum due to compression by the root of the mesentery, in a 16-year-old male teenager with a history of two previous laparotomies, which initially made us think in a bowel obstruction by adhesions; making delay on the diagnosis and definitive treatment. We review the world literature, emphasize the clinical and imaging characteristics that allow us to make its diagnosis and discuss the different treatment modalities and their results. RCM 2019; 147 (2): 43-48.
Key words: Wilkie’s syndrome, vascular compression of the duodenum, superior mesenteric artery syndrome, obstruction duodenal.
Presentamos un caso de obstrucción parcial de la tercera porción del duodeno debido a compresión por la raíz del mesenterio, en un adolescente masculino de 16 años con antecedentes de dos laparotomías previas, lo que inicialmente nos hizo pensar en una obstrucción intestinal por adherencias; lo que retrasó el diagnóstico y el tratamiento definitivo. Revisamos la literatura mundial, enfatizamos las características clínicas y de imagen que permiten hacer su diagnóstico y discutimos las diferentes modalidades de tratamiento y sus resultados. RCM 2019; 147 (2): 43-48.
Palabras clave: Sindrome de Wilkie, compresión vascular del duodeno, sindrome de la arteria mesentérica superior, obstrucción duodenal.
Email: [email protected] | [email protected]
The constriction of the horizontal part of the duodenum by the root of the mesentery or Wilkie’s syndrome (1-2), also known as vascular compression of the duodenum (3), produces a partial or total obstruction of the third portion of the duodenum, and it is manifested by abdominal pain, vomiting, loss of weight, and sometimes abdominal distension. It is an uncommon entity, which can compromise the patient’s life. For being infrequent it is not included in the initial diagnostic possibilities, which delays the diagnosis and appropriate treatment.
In this paper, we present a case in a 16-year-old male teenager, with a review the world literature, and we emphasize the clinical and imaging characteristics that allow to make its diagnosis. In our country, we found 6 publications (3-8) on this topic, which together collect a total of 7 cases.
The patient (CJ, 135866), a sixteen year old boy, with a history of 2 laparotomies, at 4 years of age for polytrauma with liver injury and at 10 years of age for adherent syndrome plus appendectomy, presented with abdominal pain, bilious vomiting on 20 occasions and radiological findings of partial intestinal obstruction Figure 1.

On examination the patient appeared ill. His weight and height were 51 kg and 1.74 mt. He refers to the loss of 4 Kg in a month. A diagnosis of obstruction of the gastrointestinal tract by adhesions was made and in the laparotomy, multiple adhesions were found in the jejuno and ileon that obstructed the intestinal transit. Adhesions lysis was performed. Patient in the postoperative refers abdominal pain. A CT scan with contrast was performed demonstrating progression of the contrast until the rectal ampulla, treatment was established for a functional intestinal obstruction, paralytic ileus, without improvement; reason why intestinal transit was performed that showed a partial intestinal obstruction between the third and fourth portion of the duodenum Figure 2a and 2b.


The patient was underwent a laparotomy on 01-09-2012, and the intraoperative findings were: extensive adhesions between loops of small bowel that obstructed intestinal transit and a conglomerate of loops of small bowel on the horizontal portion of the duodenum without appreciating dilatation of the inframesocolic duodenum. We perform lysis of adhesions, and an intestinal plication using the Noble Operation technique. In the night of 01/13/2012 and early in the morning of 01/14/2012, the patient presented abundant vomiting of bilious color. The radiography of the abdomen performed shows dilatation of small bowel loops with air-fluid levels in the epigastrium and mesogastrium Figure 3.

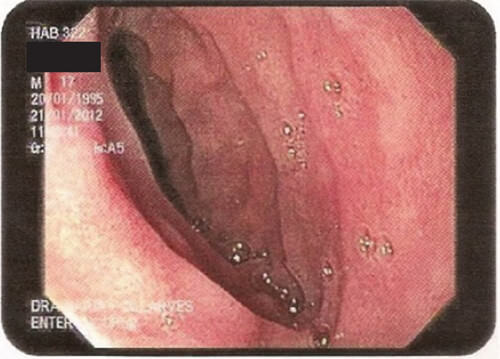
A Salem catheter was placed into the stomach and 1300 cc of bilious content was obtained. The patient was evaluated by the gastroenterology service that indicated treatment with prokinetic drugs; the bilious residue persisted in a volume of 2000 cc daily, despite treatment with prokinetic drugs. As of 01/20/2012, the patient had fever, attributed to the colonization of the catheter through which he received parenteral nutritional support. On 01/21/2012, an enteroscopy was performed, finding a narrowing between the third and fourth portion of the duodenum that did not allow the endoscope to pass through. Figure 4.
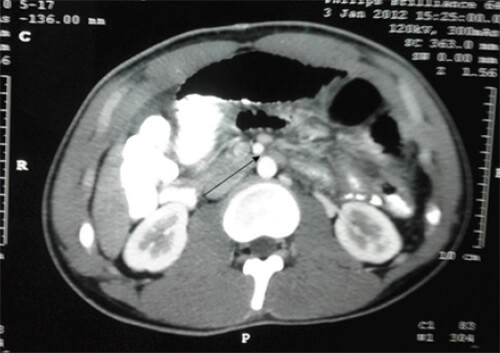
We reviewed computerized axial tomography (TAC) and observed a decreased in angle and distance aortic mesenteric, with compression of the third portion of the duodenum. Figure 5.
With the diagnosis of vascular compression of the horizontal part of the duodenum, we performed a laterolateral antecolic duodenojejunostomy, of the first jejunal loop to the descending part of the duodenum. Patient on the ninth postoperative day of the last surgical intervention, afebrile and tolerated oral feeding, we decided to discharge.
The constriction of the horizontal part of the duodenum by the root of the mesentery or Wilkie’s syndrome (1-2), also known as vascular compression of the duodenum (3), produces a partial or total obstruction of the third portion of the duodenum, and it is manifested by abdominal pain, vomiting, loss of weight, and sometimes abdominal distension. It is an uncommon entity, which can compromise the patient’s life. For being infrequent it is not included in the initial diagnostic possibilities, which delays the diagnosis and appropriate treatment. Most of the literature indicates that Rokitansky between 1842 and 1861 was the first to describe this entity (9-10), but Bermanski (11) who performed a very complete review of the Historical Background, indicates that: 1.- the first description of the superior mesenteric artery syndrome was made by Boernerus in 1752; 2.- Rokitansky in 1842, described the acute dilatation of the stomach resulting from compression of the duodenum by the root of the mesentery. 3.- Stavely in 1910 was the first to practice a successful duodenojejunostomy in a patient with gastro-mesenteric ileus. But it is not until 1921 when Professor Wilkie (1) publishes with the chronic duodenal ileus title, a series of 4 patients with three deaths and post-morten analysis and makes a very complete description of this entity and among the conclusions it should be noted that: 1.- Chronic duodenal ileus from compression of the third part of the duodenum by the root of the mesentery is a clinical and pathological entity and 2.- that the drainage of the dilated duodenum by duodenojejunostomy is the most certain method of treatment, and the only one suited for well-developed and late cases. Subsequently In 1927, Professor Wilkie published a series of 75 patients (2) and in 64 duodenojejunostomy was performed with three deaths and with satisfactory results in 80.70% of cases. After these two publications, the compression of the horizontal portion of the duodenum by the root of the mesentery is known worldwide as Wilkie’s Syndrome.
The incidence of vascular compression of the duodenum is low, between 0.0024% and 0.53% (12). It occurs most frequently in female sex and in children and young adults. In the etiopathogenesis of this disease are distinguished predisposing and precipitating factors (13). The predisposing factors are: an abnormally acute aortomesenteric vascular angle with a short superior mesenteric artery, abnormally high fixation of the duodenojejunal angle by the Treitz ligament, exaggerated lumbar lordosis, unusually low origin of the superior mesenteric artery, supine position, variations in the location of the horizontal portion of the duodenum (14); and the precipitating factor is the marked decrease in body weight with loss of mesenteric and retroperitoneal fat, which reduce the angle and the distance aortic mesenteric from its normal values from 28º to 65º and from 10 to 34 mm, at an angle less than 22º and a distance less than 10 or 8 mm (15), which produces the compression of the horizontal portion of the duodenum. In normal persons, the average of the aortic mesenteric angle ranges from 60º to 45º with an average of 56º, while the measurements of the persons with vascular compression of the duodenum vary between 10º to 22º, with an average of 14.67º (14).
Vascular compression of the duodenum is clinically manifested by post-pandial fullness, abdominal pain, vomiting, weight loss and sometimes abdominal distention (12,16-18). The clinical manifestation depends on the degree of duodenal obstruction. When the degree of obstruction is slight, the symptoms are postpandrial fullness, nausea, and sometimes vomiting that may not contain bile, and when the degree of obstruction is greater appear: the abdominal pain located in the epigastrium and vomiting with biliary contents, that can be incoercible. Abdominal distention occurs in intense degrees of obstruction and is a manifestation clinical of a severe gastric dilatation.
For being infrequent, initially the attending physician does not think about it, which delays diagnosis and treatment. The diagnosis is made by radiological studies, endoscopy and computed axial tomography and requires a careful evaluation and high index of suspicion. The radiography of the abdomen standing can show dilatation of the stomach and duodenum with few gas in the distal intestine to the point of obstruction (19), Fig. Nº 1, or a massive dilatation of the stomach and proximal duodenum, with absence of gas distal to the point of obstruction in the duodenum (20). The radiological study of the gastrointestinal tract shows: 1.- the narrowing of the horizontal part of the duodenum over the spine or to the right of the spine (21), Fig Nº 2a y 2b, 2.- few contrast and gas in the intestine distal to the point of obstruction, 3.- gastroduodenal dilatation with delay in the emptying of the contrast and fight sign of the stomach, Fig. Nº. 2a-b. Normally, the second portion of the duodenum empties the barium so quickly, that it is difficult to obtain a radiograh that shows the descending portion of the duodenum well distended. In patients with vascular compression of the duodenum, this portion of the duodenum remains distended (19) Fig Nº 2b. The endoscopy of the upper digestive tract shows the narrowing of the horizontal part of the duodenum Fig. 4. The axial and reconstructed images of the computed tomography allow: 1.- to demonstrate gastroduodenal dilatation with a narrowing of the third portion of the duodenum between the superior mesenteric artery and the aorta, 2.- to determine the value of the angle and the distance aortic mesenteric and 3.- to rule out other causes of intestinal obstruction (15,22). There are discrepancies in the publications on the normal values of aortic mesenteric angle (15,22-23), reporting as normal, values between 28º and 65º; and it is consider abnormal when it is less than 25º (15,22-23). The aortic mesenteric distance in normal people varies between 10 and 34 mm and it is considered abnormal when it is less than 8 to 10 mm (15,23).
The treatment of vascular compression of the duodenum depends on the grade of the obstruction and the patient’s tolerance. A group of patients respond to medical treatment while others require surgical treatment (24). Medical treatment consists of gastric decompression and nutritional support. Successful nutritional support using a naso jejunal feeding tube inserted endoscopically that exceeded the obstruction has been reported (25). Medical treatment is successful in 78.1% of cases (26). The surgical treatment is indicated, when the medical treatment is not successful (26-27) or when there is clinical manifestations of intestinal obstruction. There are several modalities of surgical treatment: 1.- duodenojejunostomy (1,2,27); 2.- section of the suspensory muscle of the duodenum with descent of the horizontal portion of the duodenum (28); and 3.- duodenal derotation (29). 4.- gastrojejunostomy is not recommended because the contents of the duodenum (biIe and pancreatic juice) before of the obstruction, needs to regurgitate to the stomach, to be drained into the jejuno (30,31).
In the surgical intervention, sometimes, it is not appreciated dilatation of the duodenum nor the area of obstruction, as it happened in our case, and is useful to show the level of obstruction, the insufflation of 150 to 200 cc of air through a nasogastric tube (30,31).
The surgical treatment most frequently practiced is that proposed by Professor Bloodgood (32) and popularized by Professor Wilkie (1,2), the laterolateral duodenojejunostomy.